The hip joint is the largest joint in our body.It has a hinge configuration that allows movement in different planes.At the same time, there are strong ligaments and muscles surrounding the joints.The hip joint bears the main load when walking, running or carrying heavy objects.Hip joint disease (another name for hip arthropathy) is common in both older and younger adults.Once it begins, it may go undiagnosed for a long time because significant limitations in hip movement do not occur immediately.
Often, patients begin treatment for lumbosacral osteochondrosis or knee arthrosis without any apparent results without being examined by a doctor or without presenting all complaints.Meanwhile, the untreated disease can progress and cause lameness, persistent pain, shortened legs, and an inability to bend and extend.Treatment at this stage can only be through surgery, which means that the joints must be replaced with prostheses.
Causes of Hip Arthropathy
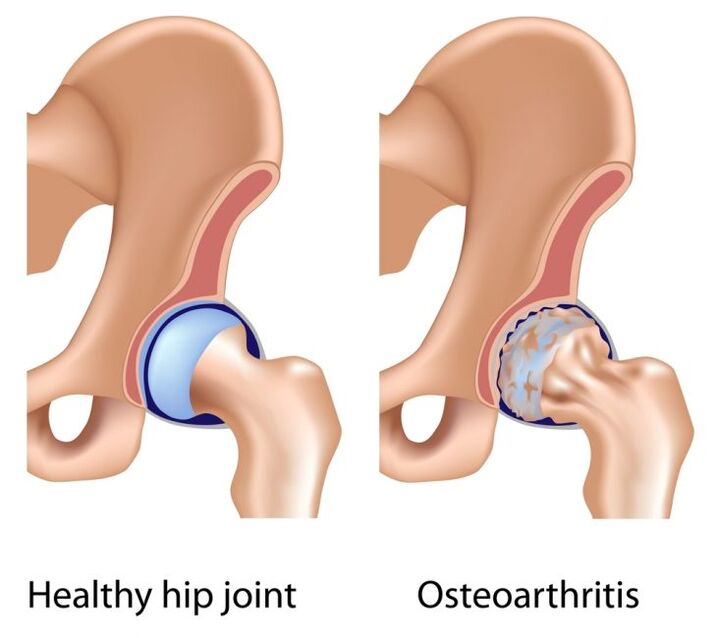
Primary hip arthritis is more common in people over the age of 40.The reasons for this have not yet been studied.The hyaline cartilage that covers the joint surface and provides sliding begins to thin and collapse.Bone spurs develop on bones due to increased friction and pressure on the bones.Joint deformation and limited movement.In primary hip arthropathy, the knee joint and spine are often affected.
Secondary arthropathy occurs in the context of a variety of diseases:
- Hip dysplasia.This term refers to congenital underdevelopment of various parts of this joint in children.As a result, the femoral head is not centered in the acetabulum as it should be.Dysplasia can be divided into three types: anterior hip dislocation, subluxation, and dislocation.With congenital dislocations, the femoral head lies outside the glenoid fossa, and without appropriate treatment, arthropathy can ensue.
- Aseptic necrosis.Because the blood supply is compromised, the bone tissue in the femoral head begins to dissolve.The bone tissue is partially absorbed and the joint head is deformed.Secondary development of joints.
- Legg-Calvé-Perthes disease.This is osteochondrosis of the femoral head, which occurs most frequently in children aged 3 to 14 years, mainly boys.Usually, it occurs as a result of complications after infectious processes, as well as injuries, physical overload and metabolic diseases.The cartilage area of the head has poor blood supply, causing necrosis of the area and deformation of the joints.
- Inflammation, infection.If arthritis occurs in the hip joint, the synovial fluid loses its lubricating properties, the inner wall of the joint thickens, the hyaline cartilage is subjected to mechanical stress, and metabolic disorders occur within the joint.
- Injuries: Bruises, femur fractures, acetabulum fractures, hip dislocations, chronic trauma, also known as systemic microtrauma.
- Hip overload associated with sports and occupational activities.For example, long periods of walking without rest, vibration effects, constant jumping, and carrying heavy objects are all bad for the joints.Muscle corsets for children or teenagers are not always able to compensate for such loads.
- With weight gain, especially at a young age, the cartilage is not yet able to support large axial loads.In addition, such patients often have metabolic problems.
- The hip joint itself is not hereditary, but inherited relatives may have certain cartilage tissue structure and metabolic disorders, which may lead to joint disease.Therefore, it is worth considering whether a parent or more distant relative suffers from joint disease.
- Osteoporosis.A common site for this disease is the femoral neck.Its structure becomes thinner and pathological fractures may occur.All these secondary causes arthropathy.
- diabetes.In this case, arthropathy occurs due to vascular disease.
- Polyneuropathy is associated with impaired sensation in the legs.
- Diseases of other parts of the musculoskeletal system.These include: scoliosis, joint and knee injuries, flat feet.The load distribution on the hip joint changes, shock absorption decreases, and the cartilage coating becomes damaged.
Symptoms of Hip Arthropathy

To prevent this disease and diagnose it early, it is important to know the signs of early arthrosis of the hip (stage 1 hip arthrosis):
- Pain that occurs periodically after physical activity.Specific pain may be localized in the groin area, sides, hips, or knees.They leave after the break, so they are not valued.At the same time, it's an alarming sign.
- Hip rotation (inward and outward) is slightly limited.You can easily check this by lying on your back and rotating your entire leg clockwise and counterclockwise.
- X-rays may show slight uneven narrowing of the joint space.
In the second stage of arthropathy, the symptoms are more pronounced:
- Pain occurs in the protrusions of the joint, most commonly in the inguinal fold, and may also occur at rest.
- Restrictions occur not only when turning the legs, but also when abducting the hips to the side.Movement of the joint is somewhat painful, especially in extreme positions (maximum abduction of the hip, bending the leg toward the stomach).
- On an X-ray, you can see moderate narrowing of the joint space and isolated bony growth on the rim of the acetabulum.Cysts may also form in the bony structure of the femoral head.
Stage III hip arthritis is easy to diagnose and its symptoms are severe:
- Joint pain when exercising at night.
- Lame, patients often use crutches.
- Joint movement is significantly limited, making it difficult to put on socks or shoes.
- The legs become thinner due to atrophy of the thigh and calf muscles.The muscles in the hip area also weaken.
- Shortening of the leg is possible due to incomplete extension and deformation of the femoral head.As a result, lumbar scoliosis (side curvature) develops and pain occurs in the lumbosacral region.
- Symptoms of stage 3 on X-rays are significant narrowing of the joint space until it disappears completely, bone growth, and deformation of the head and neck of the hip joint.
diagnosis
In diagnosis, it is important to clarify subjective complaints, collect past history, evaluate symptoms, and establish staging (radiography, CT, and MRI).Computed tomography allows you to study the bony structure of the hip joint in detail, and magnetic resonance methods can reveal the condition of the soft tissue, joint capsule, and the presence of synovitis.
treat
Treatment of hip arthrosis depends on the stage of the process and, in most cases, includes a series of surgeries.Of course, the earlier you start treatment, the better the results.
- Conservative treatment
- Medication.To relieve pain, NSAIDs are used in the form of tablets, suppositories, or intramuscular injections.Because the hip joint is surrounded by large muscles and subcutaneous tissue, dosage forms such as ointments, gels, and creams are not effective enough.Long-term use of NSAIDs is not recommended due to side effects on the cardiovascular system and gastrointestinal tract.To help them, your doctor may prescribe medication to relieve muscle spasms - a type of muscle relaxant.If inflammation is severe, intra-articular corticosteroid injections may be needed.Chondroprotectants are one of the main treatments for hip joint disease.They can be administered by intramuscular and intra-articular injection; in milder cases, tablets may be taken.These drugs are designed to improve the repair process of cartilage tissue and slow down its degradation.Your doctor may also prescribe vascular medications to improve local blood circulation.
- physiotherapy.Her surgery improved blood flow to the joint area and relaxed the muscles.These are UHF, magnetic therapy, laser therapy, electrodynamics, electrophoresis.Purpose - Based on individual indications.
- Therapeutic massage.Indispensable in the treatment of hip joint disease: relieves muscle spasms, has a beneficial effect on blood circulation and, when done systematically, strengthens muscles.
- Therapeutic gymnastics.Improves blood flow and strengthens muscle bundles in joints.Recommended exercises for hip arthritis (performed on a sturdy support):
- The "bicycle" is in a supine position;
- Lie on your back, grab your knee with your hands and pull it toward your abdomen, do the same with the other leg;
- Lie on your back, bend your knees, press the soles of your feet to the floor, lift your pelvis, and maintain this position;
- Lie on your back and move your thighs to one side as far as possible;
- Sit on a chair and squeeze the ball between your thighs;
- Lie on your back and turn your legs in and out;
- Stand with your right foot slightly elevated, hold the support with both hands, swing your left leg back and forth, left and right, and then switch legs to do the same action.
- surgical treatment.Endoprosthesis, the replacement of a joint with an artificial joint, is performed in the third stage of hip arthrosis, in the presence of limb shortening, persistent pain and severe contractures.Endoprostheses may be cemented (in the presence of osteoporosis) or cementless.The prosthesis itself can be monopolar (replacement of only the head) or omnipolar (replacement of both components).The day after the operation, some exercise therapy was carried out while lying in bed, the patient could stand, but now his legs did not need to be supported, and a few days later - crutches were needed.After 2-3 months, crutches will no longer be needed and full weight bearing on the leg will be allowed.It is recommended that patients undergoing prosthetic implants receive rehabilitation that includes physical therapy, massage, and physiotherapy.In most cases, limb function can be restored.The lifespan of a prosthetic limb is 10 to 20 years, and then it is replaced with a new one.
Prevent hip joint disease
Precautions are important, especially if you have a history of hip dysplasia, fractures, severe bruising, or suppuration in the area.
- Avoid heavy lifting and jumping (especially from heights).Try not to stand for long periods of time.
- Control your weight (reduce the intake of flour, salt, sweets, strong tea and coffee in your diet).Being overweight increases the risk of hip disease.
- Quantitative physical exercise (cycling or exercise bike, swimming, therapeutic exercises) aimed at strengthening the thigh and buttock muscles.
- If there are diseases related to metabolism (diabetes, atherosclerosis), they must be compensated.
Adherence to preventive measures, early detection of hip joint disease, and adequate treatment are keys to a positive prognosis for this disease.
Which doctor should I contact?
If you experience leg or hip pain, you should consult your doctor.He will prescribe the main diagnostic measures, specifically X-rays of the hip joint.Once the stage of the disease is determined, the patient will be referred to a rheumatologist or orthopedic surgeon.Nutritionists and endocrinologists can provide additional help in losing weight and slowing the progression of the disease.For women, it is useful to consult a gynecologist to prescribe hormone replacement therapy to prevent osteoporosis.
























